Rural residents face unique challenges when it comes to accessing quality, comprehensive cancer care which has greatly impacted their ability to lead a healthy life. For example, rural communities typically have limited access to cancer care specialists, relying on primary care providers for their care. Despite having a lower incidence of cancer in these areas, this lack of access to specialized cancer care has caused a higher cancer mortality rate in rural America. However, telehealth can be an effective way to improve access to cancer-related care for rural patients, from prevention to survivorship.
The National Cancer Institute characterizes the cancer care continuum as shown below:
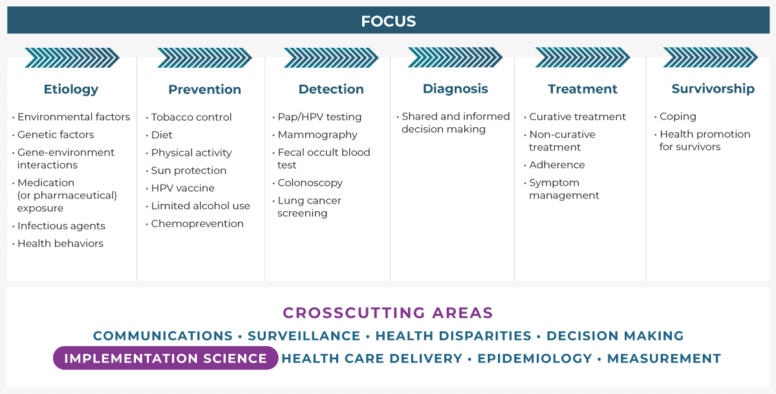
It is important that patients are provided with expert care throughout the cancer care continuum. While rural Americans face many unique challenges in receiving the expert care that is needed, telehealth can provide the following advantages for both rural patients and healthcare providers:
- Virtual visits– facilitates a visit with a provider through video or telephone without an in-person appointment
- mHealth– use of applications on mobile or wearable devices to promote healthy behaviors, monitor symptoms, or other purposes
- Remote patient monitoring– allows for remote monitoring of acute or chronic conditions or symptoms (e.g., weight loss or gain)
- Tele-mentoring– enables providers, particularly in remote areas, to connect with specialists to receive training, education, and support to best meet the needs of their patients
- Store-and-forward– an asynchronous means of sending electronic information (e.g., imaging) from one provider to another for evaluation
These life-saving advantages can be seen across the cancer care continuum in the following ways:
Prevention: Through a telehealth virtual visit of mHealth interactions, patients can receive education or counseling on tobacco prevention and cessation, diet, and other cancer prevention messages.
Screening/Detection/Diagnosis: While cancer screening such as colonoscopies and mammograms need to be performed in person, there is an opportunity to have shared decision-making conversations about screening, such as those shared decision-making visits required before lung cancer screening. Other types of screening such as skin cancer screening can be done through telehealth, and providers can have conversations about non-colonoscopy colorectal cancer screening, such as FIT, that can be mailed to the patient’s home and subsequently mailed to a lab for processing and testing.
Treatment: While surgery, chemotherapy, and radiation treatments cannot be delivered via telehealth, follow-up and other types of cancer care visits can be delivered via telehealth often at lower costs to the patient than in-person visits. A study from the Moffitt Cancer Center conducted during the COVID-19 pandemic found that the use of telehealth was associated with an average indirect cost savings of $147 and $186 per visit, including travel expenses and lost income due to missing work. Additionally, telehealth can facilitate bundling of services by allowing for store-and-forward of imaging and other information to different specialists who are part of the care team. Through Project ECHO, primary care doctors, nurses, and others can provide specialty care to their patients through a hub-and-spoke knowledge-sharing network facilitated by multi-point videoconferencing.
Survivorship: Studies have shown that telehealth can be leveraged to help patients manage the physical and psychosocial effects of cancer and its treatment, particularly around reducing fatigue, improving cognitive function, and enhancing quality of life. Additionally, patients typically report being highly satisfied with the care that they receive via telehealth.
As we search for ways to provide easy-to-access, high-quality cancer care, telehealth can be an important way to help address patient needs across the care continuum. For more information on how you can implement evidence-based and promising telehealth practices in your community, see the Rural Health Information Hub’s Rural Telehealth Toolkit. This toolkit provides resources on developing, implementing, evaluating and sustaining telehealth programs in rural communities.
Whitney Zahnd
Whitney Zahnd, PhD is an assistant professor at the University of Iowa's Department of Health Management and Policy and full member of the Holden Comprehensive Cancer Center. Her research employs health services research, social epidemiological, and spatial methods to address rural cancer disparities across the cancer continuum and to evaluate access to health care services. She has a particular interest in reducing cancer disparities among rural minority populations. Dr. Zahnd serves on the board of the Iowa Rural Health Association.